A cornea transplant replaces diseased or scarred corneal tissue with healthy tissue from an organ donor.
There are two main types of cornea transplants: traditional, full thickness cornea transplant (also known as penetrating keratoplasty, or PK) and back layer cornea transplant (also known as endothelial keratoplasty, or EK).
A graft replaces central corneal tissue, damaged due to disease or eye injury, with healthy corneal tissue donated from a local eye bank. An unhealthy cornea affects your vision by scattering or distorting light and causing glare and blurred vision. A cornea transplant may be necessary to restore your functional vision.
Corneal eye disease is the fourth most common cause of blindness (after cataracts, glaucoma andage-related macular degeneration) and affects more than 10 million people worldwide.*
When Do You Need a Cornea Transplant?
A healthy, clear cornea is essential for good vision. If your cornea is damaged due to eye disease or eye injury, it can become swollen, scarred or severely misshapen and distort your vision.
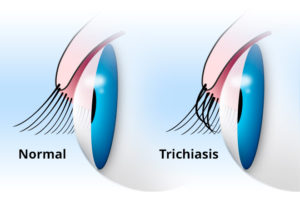
A corneal transplant might be required in cases
of conditions such as trichiasis, where eyelashes
turn inward and rub against the surface of the eye,
causing scarring and vision loss.
Certain conditions can affect the clarity of your cornea and put you at greater risk of corneal failure. These include:
- Scarring from infections, such aseye herpesor fungal keratitis.
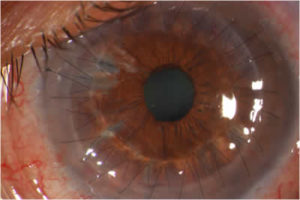
- Scarring from trichiasis, when eyelashes grow inwardly, toward the eye, and rub against the cornea.
- Hereditary conditions such asFuchs’ dystrophy.
- Eye diseases such as advancedkeratoconus.
- Thinning of the cornea and irregular corneal shape (such as with keratoconus).
- Rare complications fromLASIK surgery.
- Chemical burns of the cornea or damage from aneye injury.
- Excessive swelling (edema) of the cornea.
- Graft rejection following a previous corneal transplant.
- Corneal failure due tocataract surgery complications.
Are You a Cornea Transplant Candidate?
A cornea transplant is performed to improve the function of the cornea and improve vision. If pain is caused by a significantly diseased or damaged cornea, a cornea transplant may relieve that symptom.
With these factors in mind, you also should consider several important questions before you decide to undergo a corneal transplant:
- Does your functional vision impede your job performance or your ability to carry out daily activities?
- Can your vision be corrected with specialcontact lensesor other less invasive measures?
- How will the cost of cornea transplant surgery affect your financial situation if yourvision insurance does not cover everything from pre-screening to post-operative consultations?
- Are you able to take enough time off from work or school (up to six months to a year in some cases) to recover properly?
All of these questions, in conjunction with a thorough screening and consultation with your eye doctor, must be carefully considered before you make the final decision to have a corneal transplant.
Before the Procedure
Once you and your eye doctor decide a cornea transplant is the best option for you, your name is placed on a list at a local eye bank. You may need to wait a few days to weeks for suitable tissue from a donor eye to become available for a corneal transplant.
Before a donor cornea is released for use in transplant surgery, it is checked for clarity and screened for the presence of any diseases such as hepatitis and AIDS, in accordance with the Eye Bank Association of America’s strict medical standards and FDA regulations.
Only corneas that meet these stringent guidelines are used in corneal transplant surgery to ensure the health and safety of the graft recipient.
During the Cornea Transplant
Your eye surgeon will first administer both local or general anesthesia, depending on your health, age, eye injury or disease, and whether or not you prefer to be asleep during the procedure.
If local anesthesia is used, an injection is made into the skin around your eye to relax the muscles that control blinking and eye movements, and eye drops are used to numb your eye. You will be awake during the procedure and most people don’t report any discomfort.
After the anesthesia has taken effect, an instrument called a lid speculum is used to keep your eyelids open. Your surgeon then measures the affected corneal area to determine the size of the donor tissue needed.
Traditional corneal transplant surgery. During traditional corneal transplant surgery, or penetrating keratoplasty (PK), a circular button-shaped, full-thickness section of tissue is removed from the diseased or injured cornea using either a surgical cutting instrument called a trephine or a femtosecond laser.
A matching “button” from the donor tissue is then positioned and sutured into place. The sutures (stitches) remain in place typically for a year or more after surgery.
Lastly, a plastic shield is placed over your eye to protect it during healing.
Penetrating keratoplasty surgery generally takes one to two hours and most procedures are performed on an outpatient basis, meaning you can go home a short while after the surgery (though you will need someone to drive you home).
DONATING EYE TISSUE
Who Can Be a Corneal Tissue Donor?
How old is too old to donate eye tissue for a corneal transplant?
A decade ago, it was common for surgeons to reject corneas from people over 65 years old. But the Cornea Donor Study has concluded that corneas from people aged 34-71 are likely to remain healthy for most recipients after 10 years, with a success rate of 75 percent.
Donor cornea sutured in place of a removed cornea.
Since corneas from people under age 34 do perform better in corneal transplants, it has been suggested that younger people should receive these younger corneas.
Endothelial keratoplasty. In the past decade, a newer version of corneal transplant surgery called endothelial keratoplasty (EK) has been introduced for certain corneal conditions.
Endothelial keratoplasty selectively replaces only the innermost layer of the cornea (endothelium) and leaves the overlying healthy corneal tissue intact. The endothelium controls the fluid balance in the cornea, and if it becomes damaged or diseased, this can cause significant corneal swelling and loss of vision.
In EK, the surgeon makes a tiny incision and places a thin disc of donor tissue containing a healthy endothelial cell layer on the back surface of your cornea. An air bubble is used to position the new endothelial layer into place. The small incision is self-sealing and typically no sutures are required.
The most common type of EK procedure is called Descemet’s Stripping Endothelial Keratoplasty, or DSEK. The American Academy of Ophthalmology in 2009 endorsed DSEK as superior to the conventional full-thickness corneal transplant procedure (penetrating keratoplasty) for better vision outcomes and stability, as well as fewer risk factors.
Endothelial keratoplasty has several advantages over full-thickness penetrating keratoplasty. These include: faster recovery of vision; less operating time; minimal removal of corneal tissue (and therefore less impact on the structural integrity of the eye and less susceptibility to injury); no related suture complications; and reduced risk of astigmatism after surgery.
Within a relatively short period of time, the EK corneal graft procedure has become the preferred technique for patients with Fuchs’ dystrophy and other endothelial disorders of the cornea. However, traditional full-thickness PK is still the most appropriate option when the majority of your cornea is diseased or scarred.
Recovering From a Cornea Transplant
Total cornea transplant recovery time can be up to a year or longer. Initially, your vision will be blurry for the first few months — and in some cases may be worse than it was before — while your eye gets used to its new cornea.
As your vision improves, you gradually will be able to return to your normal daily activities. For the first several weeks, heavy exercise and lifting are prohibited. However, you should be able to return to work within a week after surgery, depending on your job and how quickly your vision improves.
Steroid eye drops will be prescribed for several months to help your body accept the new corneal graft, as well as other medications to help control infection, discomfort and swelling. You should keep your eye protected at all times by wearing a shield or a pair of eyeglasses so that nothing inadvertently bumps or enters your eye.
If stitches were used in your surgery, they usually are removed three to 17 months post-surgery, depending on the health of your eye and the rate of healing. Adjustments can be made to the sutures surrounding the new corneal tissue to help reduce the amount of astigmatism resulting from an irregular eye surface.
As with any type of surgery, always follow the instructions of your eye surgeon to help minimize corneal transplant complications and expedite healing.
Cornea Graft Rejection
Cornea transplants are performed routinely and have a reasonable success rate. In fact, cornea grafts are the most successful of all tissue transplants.
Like any other surgical procedure, a cornea transplant comes with certain risks. But, for most people, having their vision improved or restored outweighs the potential complications associated with cornea transplant surgery. It is a very personal decision for a patient to decide to undergo cornea transplant surgery.
Complications of a corneal transplant can be significant and can include cornea graft rejection,eye infection and problems associated with the use of stitches.
Rejection of the donor tissue is the most serious complication after a corneal transplant and occurs in 5 to 30 percent of patients. Transplant rejection is when your body’s immune system detects the donor cornea as a foreign body and attacks and tries to destroy it.
Research** indicates that having glaucoma and corneal swelling associated with previous cataract surgery can increase your chances of cornea graft rejection.
Recognizing the main warning signs of corneal transplant rejection is the first step to preventing graft failure. These can be remembered using the acronym RSVP:
- Redness
- ExtremeSensitivity to light
- DecreasedVision
- Pain
Rejection signs may occur as early as one month or as late as several years after surgery. Your eye doctor will prescribe medication that can help reverse the rejection process. If detected early, the graft will be successful 9 out of 10 times, according to the Cornea Research Foundation of America.
Should your graft fail, corneal transplant surgery can be repeated. While repeat surgery generally has good outcomes, overall rejection rates increase with the number of corneal transplants you have.
Vision after a Cornea Transplant
Your eyesight should gradually improve a few weeks after a corneal graft, but it could take anywhere from a couple of months up to a year to have stable vision in the eye that receives the donor tissue.
You will be left with a degree of myopia(nearsightedness) and astigmatism, because the curve of the new corneal tissue can’t match exactly the curve of your natural cornea.
Post-surgery refraction is somewhat unpredictable, and large amounts of astigmatism will still present a challenge when fitting those patients with glasses afterwards.
Mild refractive errors caused by corneal transplant surgery can be corrected with glasses; otherwise contact lenses are required.
Rigid gas permeable contact lenses, also known as RGP or GP lenses, and hybrid contact lensesusually are the most suitable contacts for corneal transplant patients due to the irregularity of the cornea after transplant. However, soft contact lenses often are an option as well.
Because your vision will fluctuate during the first few months following your surgery, it is advisable to wait until your eye doctor tells you your vision is stable before you fill an eyeglass prescription or are fitted for contact lenses.
After your eye has fully healed and any stitches used have been removed, you may be eligible to undergo laser eye surgery such as LASIK or PRK to improve your ability to see with or without glasses or contacts by reducing myopia and astigmatism.
